Table of Contents
GI bleeding
Upper GI bleed (UGIB)
- Upper GI bleeding can be divided into variceal and non-variceal causes, because of important differences in Mx strategies
| History | Likely cause |
|---|---|
| NSAID use, previous ulcer,systemic illness | Peptic ulcer disease/gastroduodenitis |
| Alcohol excess, chronic liver disease, spider naevi, jaundice, hepatosplenomegaly, encephalopathy, ascites | *Varices / portal hypertensive gastropathy |
| Excessive retching and vomiting prior to haematemesis | Mallory-Weiss tear |
| Weight loss, dysphagia | Stricture/malignancy |
| Chronic reflux, bisphosphonate use | Oesophagitis |
| Previous abdominal aortic aneurysm repair | Aorto-enteric fistula |
| Chronic kidney disease | Vascular ectasia |
| Recent endoscopic retrograde cholangiopancreatography | Post-sphincterotomy bleed |
| Peritonitis | Perforated ulcer |
| Cachexia/lymphadenopathy | Malignancy |
Assess Risk:
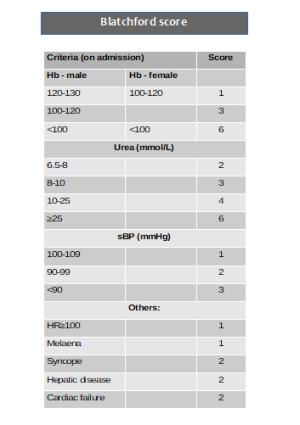
- Blatchford score at first assessment, and
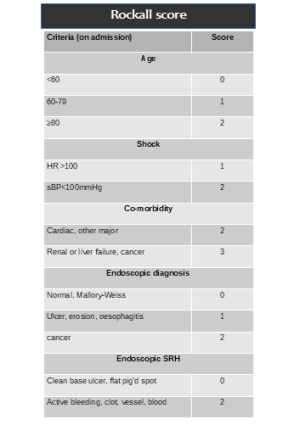
- full Rockall score after endoscopy
- A patient with a Blatchford score of 0,1 may be discharged with O/P endoscopy
- AIMS65 score (not currently used in UK) probably superior to both in predicting I/P mortality, LOS and likely ICU admission
- Score of ≥2 predicts high mortality - 1 point for each : Albumin <30, INR>1.5, alteration in mental state, sBP<90, age ≥65
Management
- Transfusion if massive bleeding with blood, platelets and clotting factors
- platelets not required if no active bleeding and haemodynamically stable.
- prothrombin complex concentrate if taking warfarin
- Do not use recombinant factor Vlla except when all other methods have failed
- terlipressin for patients with suspected variceal bleeding at presentation
- synthetic vasopressin analogue with relative specificity for splanchnic circulation
- causes vasoconstriction leading to a reduction in portal pressure
- also used in Hepatorenal Syndrome
- Dose: 1-2mg per 6/24
- prophylactic antibiotic therapy at presentation to patients with suspected or confirmed variceal bleeding.
- no evidence to support TXA in GI bleeding.
Lower GI bleeding
- Haemorrhoids
- Anal fissure
- Anorectal ulceration
- Inflammatory bowel disease (IBD)
- Coeliac disease
- Diverticular disease
- Ischaemic colitis
- Infective colitis
- Cancer (Lower GI)
- Angioectasia
- Drugs (NSAIDs, warfarin or DOACs)
- Upper GI bleeding presenting as LGIB
1st stratify as unstable vs stable: Unstable = shock index(SI) >1:
- SI is defined as heart rate (HR) divided by systolic blood pressure (SBP)
- SI greater than or equal to 1.0 was associated with 40% mortality
- SI has a normal range of 0.5 to 0.7 in healthy adults.
If stable, then risk stratify using Oakland score:
A patient with an Oakland score ≤8, is classified as a MINOR bleed and suitable for discharge from A&E and referral for outpatient colonoscopy. 6% of patients presenting with LGIB have an underlying bowel cancer, hence, endoscopy within 2 weeks is indicated in higher risk cases.
A patient with an Oakland score >8 is classified as a MAJOR bleed, and is likely to benefit from hospital admission and colonoscopy on the next available list.